|
|
|
Welcome to The Governance Institute’s E-Briefings!
This newsletter is designed to inform you about new research and expert opinions in the area of hospital and health system governance, as well as to update you on services and events at The Governance Institute.
Click here to download the full PDF version.
|
 |
|
Governance Oversight in Challenging Times: Sustaining Healthcare Board Education Remains Imperative
In recent years, the U.S. healthcare system has experienced unprecedented challenges, an increasing pace of change, and ever-growing complexity. Boards may be tempted to defer continuing education at this time, potentially out of a desire
to avoid adding to the executive team’s burdens in the midst of a public health crisis, the belief that crisis management must take priority over longer-term strategic planning or educational activities, or that board expenditures
for non-essential activities should be minimized in a time of ever-tightening margins. This article explains why placing board education on the back burner is unwise.
Read More
Collapse Article
By Anne Murphy, Partner, Arent Fox, LLP, and Liz Sweeney, President, Nutshell Associates LLC
|
Key Board Takeaways
While it may be tempting to set aside continuing education plans in the current climate, it is more critical than ever that boards are informed and diligent during this challenging time. Boards will need to:
-
Remember their legal obligation to make educated decisions on behalf of the organization. This is a core fiduciary duty. Plus, there is currently more scrutiny from the public, government, ratings
agencies, and investors, and this will continue well into the future.
-
Embrace a culture of transparency for decision making. This includes creating an environment where board members are comfortable speaking up and asking questions if they don’t feel they have adequate
information to make a knowledgeable decision.
-
Proactively take charge of education. Board leadership should develop an approach to continuing education that addresses critical, need-to-know topics for the board and should play a direct role in
organizing these educational efforts. Having appropriate education will help ensure all relevant risks and strategies are being addressed appropriately.
|
In recent years, the U.S. healthcare system has experienced unprecedented challenges, an increasing pace of change, and ever-growing complexity. These changes include the shift to value-based purchasing models, expansion of care
delivery in non-acute settings, technological advances, the growth of a consumer-empowered patient population, ongoing consolidation, and the entry of non-traditional and well-financed disruptors into the care delivery system.
The prevalence of COVID-19 has now brought the unprecedented financial and operational strain of a global pandemic into this already-dynamic environment.
Hospital and health system boards face unique challenges in this climate. Not only does the current environment require a robust board infrastructure and attention to the appropriate array of subject matter expertise and experience
of directors, but it also demands a sustained and disciplined approach to continuing board education. Boards may be tempted to defer continuing education at this time, potentially out of a desire to avoid adding to the executive
team’s burdens in the midst of a public health crisis, the belief that crisis management must take priority over longer-term strategic planning or educational activities, or that board expenditures for non-essential activities
should be minimized in a time of ever-tightening margins. Placing board education on the back burner, however, is unwise.
|
"Non-profit hospital and health system boards are the custodians of among the most complex enterprises in the world, at what appears to be the most challenging possible time in the history of healthcare."
|
In the face of competing demands for the attention of healthcare boards and executive teams, there is an inevitable need to prioritize the finite time and resources available for the governance process. This challenge is compounded
by the primarily volunteer status of boards, but it does not diminish the profound complexity of the healthcare delivery system or the fiduciary duties required of boards to oversee their organizations with diligence and informed
attention. To the contrary, these boards are the custodians of among the most complex enterprises in the world, at what appears to be the most challenging possible time in the history of healthcare.
The last several months have reminded us that the future is impossible to predict with certitude. An effective board now must provide informed direction on matters that have no historical precedent, relating to mission-critical
matters such as care delivery in a pandemic, rapid expansion of telehealth and digital care delivery, and effective application of principles of social justice and racial equity to the care provided. For many institutions,
there will be crucial decisions to be made in the near future about the strategic and financial direction of the system in light of innovations such as artificial intelligence, addressing social determinants of health (SDOH),
and new models for care delivery in the home. Further, boards and senior leaders must balance the need for surge capacity and preparation for the next wave or the next pandemic against the conflicting need for transforming
their inpatient facilities to accommodate easier access, convenience, and value in flexible care settings being demanded by today’s consumers. With the pace of decision making rapidly accelerating, boards must be educated about
key issues to make decisions in a timely way. Without it, the organization risks delaying critical initiatives or, worse, the effects of bad decisions.
The Board’s Responsibility to be Informed
From a core fiduciary perspective, a hospital or health system board has the legal obligation to exercise reasonable diligence to make informed decisions on behalf of the organization. While the board can rely upon the views of
trusted management and outside advisors in the course of exercising this responsibility, this does not alter the board’s duty to provide the sort of informed oversight that comes from a well-developed board education infrastructure.
Public interest in the healthcare delivery system is more intense than ever. As care models continue to evolve, so will the focus on the competency of governance. A board that demonstrates a disciplined education program will
be better positioned to withstand this attention. In addition, ratings agencies and investors routinely review whether a board has engaged in governance best practices, including education. The now-prevalent use of environmental,
social, and governance (ESG) criteria in the capital markets highlight the growing importance of the “G” in ESG and require a demonstrated and sustained board education program that is well-calibrated to emerging risks and
opportunities. Furthermore, the U.S. Department of Justice emphasizes the importance of continuing education in its compliance program evaluation guidance,1 including the importance of an active and informed board
oversight role in compliance and continuous improvement in management of compliance risks.
|
"Against this backdrop, healthcare boards should be vigilant about governance decision making that cannot be completed in the absence of adequate board education."
|
Against this backdrop, healthcare boards should be vigilant about governance decision making that cannot be completed in the absence of adequate board education. If, for example, the board is called upon to make a decision related to entry into a significant
risk-based contract, or to approve an investment in digital health, and believes it does not have sufficient context to make a fully informed decision, it is incumbent on the board to insist on receipt of that information before
a decision is rendered. An individual board member who does not believe he or she has adequate information to make an informed decision should speak up, and the board should embrace a culture of transparency as to whether it
is ready to make a decision.
Proactively Take Charge of Education
Because effective governance requires setting strategic direction, it must go beyond simply reacting to what is put in front of the board. Boards can proactively take charge of their education program. Such an approach arms boards
with the knowledge to ask the right questions about issues that management may not be visibly addressing. This approach retains the board’s independence and ensures all relevant risks and strategies are being addressed appropriately.
Board education can and should take place in a manner that is both time- and cost-efficient. Numerous resources are available to assist boards in these educational activities, including Webinars, on-demand e-learning, and other
technology-enabled activities that can fit into any schedule and budget. Financial and legal advisors often include periodic board education as part of their service package and have a wealth of knowledge due to their wide
visibility into capital markets, regulatory, operational, and strategic trends. Board leadership should develop an approach to continuing education that addresses topics of the greatest interest to the board and should play
a direct role in organizing these educational efforts.
Continuing board education is an essential element of healthcare oversight, now more than ever. Only with this ongoing education will the board be in a position to provide informed, independent, and proactive enterprise governance
in the context of these sea changes, reflecting the nuanced balance of business, mission, operational, financial, technological, reputational, clinical, public health, and strategic factors. In the absence of this sustained
education, the board would be limited in its ability to provide the executive team with that fiduciary direction, at the very moment in time when it is most needed. This would raise the specter of board direction that lacks
the vision to take bold action or, conversely, the failure of the board to identify inherent risks and therefore place its organization, its patients, and its community in harm’s way.
The Governance Institute thanks Anne Murphy, Partner at Arent Fox, LLP, and Liz Sweeney, President of Nutshell Associates LLC, board member at the University of Maryland Medical System (UMMS), and former Managing Director at S&P Global Ratings, for contributing this article. They can be reached at anne.murphy@arentfox.com and liz@nutshellassociates.com.
|
|
Facilitating Great Board Practices
In view of current events, now is an opportune time for all boards to review their governance processes and consider changes to them in an effort to successfully lead their institutions. This article provides guidance on how to have effective
board and committee meetings, which will help a board fulfill its fiduciary responsibilities and document that it has done so. More importantly, it will help heighten board members’ awareness of the types of issues to think about—not
only to govern the institutions they serve, but to improve the quality of the lives of the populations served.
Read More
Collapse Article
By Thomas C. Senter, Esq., Partner, Greenbaum, Rowe, Smith & Davis LLP
|
Key Board Takeaways
The following are important questions for board members to ask of themselves and each other. They should be asked to help guide future board initiatives and discussion:
-
Do we know and understand our mission? Is it the right one today? Will it continue to be the right one three or five years from now?
-
As a board, do we understand the unique needs of the populations we are here to serve?
-
Are efforts being made to ensure that the board reflects and represents the populations it serves?
-
Are we ready and able to rewrite our playbook to consider the pandemic, the Black Lives Matter movement, and other events and issues, to be responsive to today’s needs and do more than we have in the past?
-
What is our institution’s role in addressing the social determinants of health that go beyond the 15–20 percent of a population’s health that our institution can directly impact? If we do not step up and
address this issue, who will?
|
In view of current events, now is an opportune time for all boards to review their governance processes and consider changes to them in an effort to successfully lead their institutions. This article provides guidance on how to
have effective board and committee meetings, which will help a board fulfill its fiduciary responsibilities and document that it has done so. More importantly, it will help heighten board members’ awareness of the types of
issues to think about—not only to govern the institutions they serve, but to improve the quality of the lives of the populations served.
Background on Board Governance
When discussing a board governance issue, it is always helpful to review certain basic duties by way of background. These include the following: Who does the board serve? What are its responsibilities? How does it fulfill them
and how does it document the fact that it has done so?
The board owes its duty to the population served by its institution. In the case of a non-profit hospital or health system, that population is, in effect, the shareholders or owners of the institution. It is an interesting relationship
as the board owes fiduciary oversight duties and is held to a high legal standard by a population which is largely unaware of its existence.
Important duties of the board include the following:
-
Duty of care: Not only is the board responsible for oversight of the clinical care provided, they are responsible to oversee the financial resources of the institution to ensure that it is sustainable and can fulfill
its mission today and in the future.
-
Duty of loyalty: The board owes this duty to the institution, those who use its services, and the population it is there for. The duty of loyalty is undivided, and conflicts must be avoided.
-
Duty of obedience: The board must ensure that the institution’s mission continues to be the right one. If it is, be true to it. Otherwise, change it.
-
Future vision: The board is responsible for establishing long-term goals and strategies of the institution and overseeing their implementation.
These duties and others are easily stated but not always easy to carry out. It is not enough to make sure that the mission is served today. The board must be proactive and take steps to help ensure that the mission will be served
for generations to come. To do so, the board needs to understand healthcare today. However, it is equally important that they stay abreast of changes and trends in the industry. If they fail to do so, they will not be able
to effectively protect the institution for those who will need it in the future.
Board and Committee Meetings
Board and committee meeting agendas should be set, and the dialogue should be driven, with the above duties in mind. Forward-thinking and proactive boards must also do the following:
-
Deal with the basics. By way of example, these include setting agendas, reporting up from the committees to the full board, keeping accurate minutes that document the way the board fulfilled its responsibilities,
and management reporting. It is helpful to start with an annual calendar of all board and committee meetings to ensure that appropriate reporting from the committees to the full board is scheduled.1 This
calendar will also help ensure that all required board actions (e.g., approval of an audit, elections, and discussion and approval of a community health needs assessment) are covered, and make it easier to plan for
other meaningful agenda items including educational sessions and reports by clinicians, outside consultants, and management. While it is important to start with a calendar that will help ensure the board deals with
the basics, it is as important to have a fluid process over the course of a year that allows for, and encourages, the board to quickly change its course and deal with those issues that could not have been anticipated
when the calendar was set. As discussed in this article, the current pandemic is an unfortunate and great example of such an issue.
-
Take a fresh look at your playbook. Often, board chairs and secretaries will look to last year’s calendar to set one for the current year. It is an efficient and seemingly logical approach. However, if this process,
which I have been guilty of, is all that is done, it will not be enough. Think about how your institution has evolved and changed over the years. Board members must do the same. If your institution does not change with
the times, does not react to current trends in healthcare and look to the future, your institution will fail. The same holds true for your board.
-
Recognize you are the accountable ones. Do not rely on management to do your job. A critical role of successful boards is to have great CEOs. This means helping them develop, working in collaboration with them, supporting
them, letting them do their job, and making sure there is a succession plan in place. The CEO is responsible for day-to-day operations; the board is not. While the CEO should be a valuable source of information for
the board and is likely a fellow board member, you cannot rely on the CEO to do the board’s job and fulfill its fiduciary responsibility. For example, is your board doing enough to understand future trends in the industry?
Does your board know enough to make informed decisions about partnering with another organization or adding or closing certain service lines? While the right CEO will be proactive and come to the board with his or her
thinking on these issues and with information to support recommendations made, ultimately these are decisions to be made by the board that cannot be delegated to management. Remember, if your institution fails to change
with the times and consider and make prudent strategic decisions, the fault is with the board and not management.
Today, boards must be forward-thinking. To do so, most of the time at board meetings should be devoted to looking forward and discussing the future. Information on past events, including quality and patient experience scores, financial
reporting, and money raised, should be reported to the board and is important information for the board to have. However, for purposes of board meetings, they should be discussed in the context of what they mean for future
planning rather than merely as a rehash of past events.
What Have Current Events Taught Us?
We all know that healthcare has been changing at warp speed. The pandemic took an industry that was changing more rapidly than, perhaps, any other and turned it upside down. Topics that were at the forefront of our thinking as
board members earlier this year had to be temporarily pushed aside to focus on the current crisis. While management had to deal with the new challenges on the front lines, boards also had to change their focus and ask questions
that were new to everyone. These included:
-
How do we support those on the front lines when their own lives are at risk?
-
Are management, the board, and the entire institution nimble enough to address challenges that are beyond anything we have had to deal with in the past?
-
Where do we look for help outside of our institution?
-
How do we keep our non-COVID patients and staff safe when many of our beds have been converted to ICU beds and we have far more ICU patients than we do staff trained to care for them?
-
How do we manage the extraordinary loss of revenue and make sure the institution is doing what it can to get money from the government and from any other available sources?
-
How do we compensate our employees? While many of them are working harder and longer than ever before, demonstrating that they are truly working in a noble profession, do we have the resources to pay them what we think
they are worth?
-
What have we learned that will make us better prepared if there is a second wave of the COVID-19 virus or if we are confronted with a different pandemic?
-
The pandemic has made us better aware of the important role telehealth will have in providing care for our communities. Are we considering how to best use it to care for those we are here for?
While these questions and many others are often on management’s list to address and report on to the board, it is on us as directors to make sure we have the right management team in place to do so. These are difficult questions
and difficult times to deal with. Some questions may be hard to ask and all of them are hard to answer. Board members have a responsibility to raise them. Hopefully, we have strong management leaders who will bring many of
the questions to us. Whether or not that is the case, as directors, we must be well enough informed and proactive enough to raise them on our own.
We also need to have a fluid board and committee structure for management to report into. The board’s oversight and time devoted to the pandemic needs to be well documented in the minutes. Also, boards must consider not only the
current crisis caused by the pandemic, but its future impact on the health of our population. While a vaccine or other medical breakthroughs may protect us from COVID-19, the resulting behavioral health impact will have to
be addressed for years to come. Other important issues relating to our institution and the health of those we are here for, such as the Black Lives Matter Movement and health disparities between different groups, must also
be considered by forward-thinking boards. Clearly, it is not business as usual.
Conclusion
These are challenging times for boards. Motivated by a desire to help, we are charged with overseeing the future viability of, and quality of services provided by, large and incredibly complicated and important institutions. We
often must do so under a business model in which our organization’s need for financial resources is growing at a much greater rate than is our institution’s ability to accumulate the resources it needs.
Board members need to know more and do more than ever before to effectively serve. We need to be sure that our institution has the right mission. We then need to be guided by it and ask the right questions and act to be sure that
we remain true to it. Board and committee meetings should be structured and conducted with these thoughts in mind.
While these are challenging times, thoughtful and forward-thinking boards have more opportunities than ever before to positively impact the future of healthcare and the health of the communities they serve. Each major event and
issue in our society that relates to the health of those we serve, be it a pandemic, racial inequities, access to behavioral health services in our community, obesity, and others we cannot even envision today but will have
to deal with tomorrow, is an opportunity for us to throw away yesterday’s playbook, figure out how our institution can do more, and then steer and oversee the process of change for the benefit of those we serve. This is our
responsibility. While it is daunting and the stakes are very high, we should all be proud to serve and thankful for the challenges and opportunities ahead of us.
The Governance Institute thanks Thomas C. Senter, Esq., Partner in Greenbaum, Rowe, Smith & Davis LLP, for contributing this article. He is the immediate Past-Chair of the Board of Trustees of Englewood Health System and Englewood Hospital and currently serves as a member of its executive committee. His views expressed in this article are solely his own and should not be attributed to his law firm or Englewood Health System. He can be reached at tsenter@greenbaumlaw.com.
|
|
Critical Thinking and Health Services Strategy: Beware the Behavior of the Herd
Healthcare delivery systems and provider organizations have to make critical business decisions based upon emerging healthcare marketplace status assumptions and assertions that are put forward by an ever-increasing number of pundits,
leaders, and politicians. While many of these assumptions can be visionary, laudable, and even motivational, they can also be wrong. This article presents five ubiquitous, but largely unsupported, assertions about the state and future
of healthcare delivery in the U.S. Each is followed by a rebuttal, thus challenging the assertion with plausible alternative positions.
Read More
Collapse Article
By Daniel K. Zismer, Ph.D., Co-Chair and CEO, Associated Eye Care Partners, LLC, and Endowed Professor Emeritus and Chair, School of Public Health, University of Minnesota, and Gary S. Schwartz, M.D., M.H.A., Co-Chair and Executive Medical Director, Associated Eye Care Partners, LLC, and President, Associated Eye Care, LLC
|
Key Board Takeaways
U.S. health systems are under increasing financial and market dynamic pressures. The COVID-19 pandemic has revealed underlining balance sheet condition, mission plans, and organizational strategy weaknesses. While
working through these challenges and strategically planning for the future, the board should:
-
Highly question assertions about the current state of healthcare. Board members and senior leadership teams are being bombarded by theories and predictions on how healthcare markets and related delivery
strategies “should behave,” and how they should change mission strategies and business models. Many of these prevailing theories and predictions are likely to be wrong, or organizations will act far
too soon to impending change, leaving them strategically and financially vulnerable.
-
Engage in a process of collective rational thinking. A major challenge and opportunity presenting to boards and senior leaders is the discipline of rational thinking using framework questions as a
foundation for discerning how to work together to steer missions, clinical services programming, and related capital investment strategies over the next several years.
|
Healthcare delivery systems and provider organizations have to make critical business decisions based upon emerging healthcare marketplace status assumptions and assertions that are put forward by an ever-increasing number of pundits,
leaders, and politicians. While many of these assumptions can be visionary, laudable, and even motivational, they can also be wrong. Evidence shows that many U.S. hospitals are in trouble; financial operating performance is
declining, resulting in hospitals closing at an accelerating rate.1 It is unfortunate, but blind faith in the emerging “new critical thinking” has contributed to the peril of at least a few of these stories of success
that have instead failed.
A brief case vignette can help illustrate this point. RehabCare, a not-for-profit, inpatient and outpatient rehabilitation hospital in the upper Midwest, experienced significant operating economic performance erosion (see Exhibit 1).
This was partly because its operating expense inflation rate trajectory exceeded its inflation-adjusted reimbursement rate per unit of services provided over a number of years. Continuation of the trend was predictive of eventual
financial collapse and institutional closure. Success of the projected turnaround plan was contingent upon several assumptions about how the healthcare marketplace was predicted to behave. Chief among these assumptions was
the need for third-party payers to transfer substantial proportions of premium funds to health systems in the form of value-based payments. It was assumed that health systems would transfer patients to RehabCare to reduce the
length of stay in the more expensive acute-care settings within their systems. RehabCare would then be paid directly by referring hospitals out of their found profits earned from a new payment method.
Unfortunately, this was an incorrect assumption. The success of this plan was entirely dependent upon a seismic shift in how insurers and health systems would do business together. This shift did not occur. RehabCare’s financial
resources ran short, and the board determined that a merger with a larger community health system was required to prevent the organization from closing its doors.
|
Exhibit 1: A Demonstration of Economic Productivity Erosion
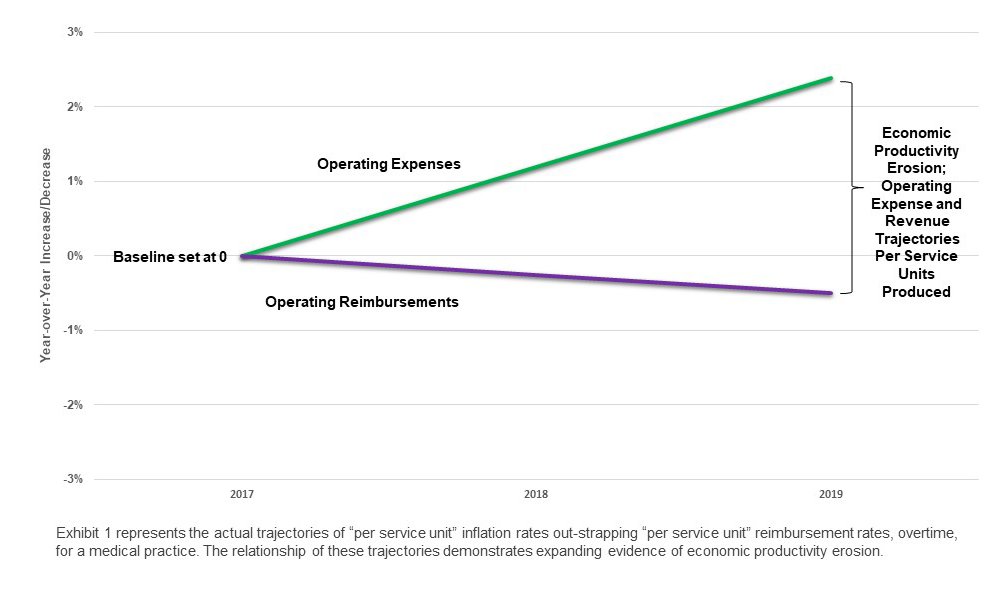
click image to enlarge
|
The balance of this article presents five ubiquitous, but largely unsupported, assertions about the state and future of healthcare delivery in the U.S. Each is followed by a rebuttal, thus challenging the assertion with plausible
alternative positions. The goal of this exercise is to encourage conversations between boards and senior leadership teams as they consider business planning and strategic positioning of healthcare services for their organizations
amidst uncertain policy and marketplace dynamics.
Five Assertions around Healthcare Delivery
|
Board To Do: Become more knowledgeable about how payer models and methods will interact with community health system strategy to affect access to patients, competitor behaviors, and organizational financial performance overall.
|
Assertion 1: Payers will change to value-based payment methods, shifting their focus from paying for the care of sick individuals to paying to maintain the health of covered populations.
Rebuttal: Major commercial and governmental payers currently work from a business model where they receive funds first in the forms of insurance premium payments, taxation transfers by governmental organizations, and revenues
earned by self-insured businesses. These payers are advantaged by the “float”2 and an ability to lever annual inflation rates on policy premiums charged. The payer side of healthcare is an ever-consolidating market
and, in most markets, five or fewer payers control the lion’s share of the payments to all medical providers, including the governmental payers (Medicare and Medicaid). In these markets, the provider side is highly competitive
and may be over-supplied, leaving providers vulnerable to price and total cost of care pressures by insurers. The payers’ incentives are to hold revenue from premium dollars as long as possible to increase the value of the
float, while exerting maximum downward pressure on unit price, number of service units reimbursed, and total cost of care.3 Consequently, so long as market dynamics favor an increasing economic spread between revenue
from premium rate inflation and reimbursements paid to providers, there is a negative incentive for transferring dollars to providers in advance of services rendered. Value-based reimbursement may expand but will likely be
an experimental science for some time to come.
Does this mean that community health systems shouldn’t consider strategies designed to work differently and productively with governmental and commercial payers? No. A number of organizations are having success with innovative
payer strategies, such as “surgical bundles,” offering fixed pricing to payers for knee replacements and other orthopedic services; entering into incentive payment opportunities for narrowing variations of total cost of care
profiles for defined chronic conditions such as heart failure management; and entering into tiered provider arrangements based upon the exchange of price and total cost of care concessions for improved and efficient access
to patients.
|
Board To Do: Be cautious about entering into strategies that don’t support the organization’s vision, require shifting clinical services designs, and completely rely on payers changing how they pay providers.
|
Assertion 2: Healthcare institutions and related medical providers should broaden their focus from treating sick individuals to maintaining the health of large population groups.
Rebuttal: By all reliable sources of evaluation, healthcare providers can influence about 20 percent of factors that determine the health status of a population.4 The factors that caregivers have little to no
control over include social determinants of health, diet, lifestyle choices, genetic predispositions, and other factors. We are not saying that this knowledge minimizes the value of the healthcare system; it does, however,
call into question whether healthcare providers are best positioned to be in the business of “population health.” Most, if not all, organizations that currently provide healthcare lack the core public health competencies, resources,
and essential, internal financial incentives alignments to be in the business of population health.5 Alternatively, people will continue to become ill and suffer trauma at predictable rates, needing to be managed
by those doctors, nurses, and other providers of healthcare who are currently educated and trained to care for the sick and broken. But, all organizations, regardless of size, can think about and begin to acquire some measure
of public health practice competencies into their organizations with careful consideration for the attendant risks of jumping into the deep end of the pool. The issue for boards and senior leadership teams is to avoid being
lured into strategies that require abrupt shifts in vision, strategy, and clinical services designs, in anticipation that payers will fundamentally redirect their methods for paying providers (e.g., away from fee-for-service
to pay-for-performance models). A fundamental question for boards and senior management is, “What business are we prepared and qualified to be in?” An even more fundamental question for those who educate and certify the frontline
providers is, “With the current and growing shortages of primary care providers, are we willing to shift the educational focus from healing the sick to managing the health of populations?”
|
Board To Dos: Work with senior leadership to:
-
Ensure you have clinical care performance scorecards that reflect clinical services outcome results that are likely to be on the radar screens of the payers.
-
Examine the incentives created by provider compensation plans. Carefully consider how plan designs create incentives that may affect the performance of strategic plans.
|
Assertion 3: Fee-for-service medicine establishes perverse incentives. Providers should be paid for outcomes instead of units of service.
Rebuttal: If we have learned anything from the discipline of medical economics, it is that any payment system can, and typically will, establish perverse incentives, and become vulnerable to fraud and abuse. All healthcare
decision makers, whether they are providers caring for an individual patient, administrators managing a healthcare system, or politicians concerned with the health of their constituents, have to weigh clinical decisions against
economics and financial incentives. In addition, everyone must then inject their own moral and ethical standards into their individual decision-making equation. In our current system of healthcare, the provider-side holds responsibility
for the bulk of this decision making. One can make the argument that our current system perversely rewards “units of care” (i.e., volume over quality). On the other hand, a fee-for-service-inclined reimbursement system would
seem to be reasonable if the right services are provided to the right patients at the right times. Every payment model and method available to the imaginations of the designers will carry some level of moral hazard. Boards
and senior leadership teams can build their clinical care performance scorecards to reflect clinical services outcome results that are likely to be on the radar screens of the payers. This includes outcomes such as adherence
to accepted clinical indications for inpatient medical and surgical admissions, third-party payer reimbursement services denial patterns, unsupported inter-provider variations on surgical and interventional device implants,
inpatient readmission rates, and clinical services coding and documentation patterns, especially for providers who function as employees of the organization.
Additionally, to the extent that community health systems employ physicians, boards and senior leaders should examine the incentives created by provider compensation plans, paying special attention to how plan designs create incentives
that may affect the performance of strategic plans. The incentives established by employed provider compensation plans exert a direct effect on health system strategy performance. Incentives influence how providers shape and
conduct their practice.
|
Board To Do: Think through the unique risks and challenges your organization is facing and always take these into consideration when strategically planning for the future.
|
Assertion 4: All providers are facing the same challenges. All are sinking in the same boat.
Rebuttal: While it is true that all providers operate within the same world of healthcare macroeconomics, not all are exposed to the same risks. Not-for-profit, tax-exempt, charitable institutions, for example, may have
constraints in the flexibility of their business plans and models due to mission commitments or legal or tax code regulations. Likewise, physicians in independent practices often live within self-stylized clinical service and
business models that have served them well in the past but are not well-positioned for the future. When those who control the revenue streams and regulatory environments disrupt the healthcare economics and policy status quo,
many providers either refuse to or are unable to adapt. The lesson here is not all healthcare providers are “in the same boat.” While each is subject to the same market and macroeconomic dynamics, business model resiliencies
differ.
Assertion 5: Demographics favor increasing demand for all health services and that is good for the business of community health systems.
Rebuttal: If the COVID-19 pandemic has taught healthcare providers anything, it is that increasing demand does not automatically translate to positive financial returns. The financial performance of every health system is
a product of the balance of the operating economics of its clinical services portfolio mix. Every clinical service and service line carries a unique operating economic performance signature. The aggregate of the economic performance
of the clinical service line portfolio dictates the overall financial performance of a community health system or large medical clinic (see Exhibit 2).
|
Exhibit 2: Health System Consolidated Clinical Service Line Portfolio Net Financial Margin Performance

click image to enlarge
|
|
Board To Do: Work with senior leadership to routinely “stress test” the risk profile of the organization’s aggregate clinical services portfolio
|
Boards, together with senior leadership, should routinely “stress test” the risk profile of the organization’s aggregate clinical services portfolio. Components of a rigorous strategic and financial stress test include, for example:
-
The ratio of inpatient to outpatient revenue productivity
-
The proportionality of revenue productivity of high-growth outpatient revenue categories of service, such as orthopedic and ophthalmologic surgical services
-
Balance sheet capacity for investments in areas of high demand and financial margin potential
-
The availability of affiliated physicians in specific, strategic service lines
-
Where the organization may be overly dependent upon clinical services at-risk for decreasing demand and reimbursements, such as inpatient orthopedics and cardiovascular care
On the payer side, the stress test addresses proportionality of payer mix and trends, and the risks of specific payers reducing reimbursement rates on higher margin services deriving from growing market power of the payers that
control larger portions of the system’s revenue flows. It is the responsibility of boards to work closely on the economic balance of the consolidated clinical service line portfolio that serves the mission of the organization.
Synthesis of the Critical Thinking Activity between Boards and Senior Leaders
So, what does all this have to do with critical thinking and rational business planning? The answer is everything. Strategic planning and resultant business plans are a combination of a little bit of science and a lot of
educated and experienced guesswork. The value of the final product is dependent upon assumptions made about the local and national healthcare environment, and these assumptions are subject to influence from a number of different
sources. The leaders’ challenge is to find the strategy and business plan path that, on a risk-adjusted basis, is most likely to yield the highest chance for success. How do leaders do that? They must engage in a process of
collective rational thinking. Here, “rational thinking” is defined as “an ongoing process of structured and disciplined decision making, based upon a systematic approach of analysis and selection of actions among available
choices, within a given set of complex, changing dynamics and environmental conditions, all in a context of what prudent, moral, and ethical leaders might do, given all the factors that pertain.” 6
To see how the definition of rational thinking comes to life as leaders create a rational strategy, and strategic plan for their organizations, let’s return to the basis for the assertions and rebuttals provided above. The purpose
of this exercise was not to carte blanche, rebut, or discredit assertions that are openly being presented by industry experts to community health system boards and leadership teams; rather, the goal is to encourage critical
thinking and debate between community health system boards and leadership teams prior to the codification and execution of strategic plans that commit organizations to actions and investments that carry potential for both reward
and risk.
To this end, a framework is offered to guide critical thinking as board members and leaders consider options for strategic investments and actions to advance the mission and goals of their organizations. This framework is designed
to guide the required, board-level discussions from a perspective of not accepting each popular assertion of how community organizations should act strategically, on their face, without first subjecting each to the test of
a rigorous, structured debate followed by clearheaded discernment and decision making. Disciplined discernment is a principal requirement of good governance. This framework is presented in the form of seven guiding questions
with illustrations.
When executed, will the strategic plan being considered:
Require us to depart significantly from our stated mission and mission responsibilities to the communities we serve? Can we draw specific connections between the new plan and established mission responsibilities?
Cause us to divert excessive amounts of financial and other organizational resources from commitments and mission-related requirements; i.e., do we risk under-resourcing existing promises and commitments made, including the
provision of capital needed by the organization to achieve high standards of performance as we operate now?
Allow room for us to recover from the financial and reputational toll exacted on the organization, including the effects on the organization’s balance sheet, if one or several goal execution strategies fail?
Require the addition of internal human resource competencies that are not resident in the organization now, and if so, who on the senior leadership team is qualified to source, evaluate, and oversee new members of the team?
In other words, do we have the right people on the senior leadership team to expand the internal competencies required of the plan?
Have effects on the culture, and the related values and belief system of the organization, that must be considered and be attended to at the highest levels of leadership as the new plan is rolled out?
Be financially affordable through the full period required to develop and operate the plan to the point where it begins to bear fruit and produce required returns on the investments made. In other words, can the organization
afford the financial “ramp-up” phase of the plan?
Cause our competitors to react in ways that need to be considered? Every strategy, by definition, is designed, in part, to advantage an organization in a competitive market. Every strategy should be expected to elicit a competitive
response.
Does the application of such a critical thinking framework mean that community healthcare organizations should not take risks with strategy? Certainly not. The point implicit in the application of the framework provided above goes
to the argument for critical thinking by boards in collaboration with senior leadership teams, including the application to critical thinking as it relates to prevailing, popular proclamations of how the U.S. healthcare system
“should behave,” which may be right at a macro level, but wrong for specific organizations at specific times.
Summary
Boards and senior management teams hold the responsibility of discernment regarding the future of the organizations they serve. In fact, discernment is a principal responsibility and required competency of governance, working hand-in-glove
with management. It is the foundation of rational decision making, and is key to enabling boards to transform their organizations in such a way that can succeed and sustain, rather than preserving the status quo or taking risks
that do not pan out and potentially put the organization in a worse position.
The first step on the path to more effective discernment is consensus among directors and senior management that an industry under pressure, such as healthcare, will inevitably precipitate pervasive speculation on what might be,
could be, or should be “next.” It is the role of governance and leadership to determine the best path through the related “noise.”
The Governance Institute thanks Daniel K. Zismer, Ph.D., Co-Chair and CEO, Associated Eye Care Partners, LLC, and Endowed Professor Emeritus and Chair, School of Public Health, University of Minnesota, and Gary S. Schwartz, M.D., M.H.A., Co-Chair and Executive Medical Director, Associated Eye Care Partners, LLC, and President, Associated Eye Care, LLC, for contributing this article. They can be reached at dzismer@aecpmso.com and gschwartz@aecpmso.com.
|
|